As we know, anything is possible in vascular surgery and vascular surgeons like to get creative at times. Also, 90% of the time patients will not be able to tell you what kind of fistula was created. Hence, as the sonographer you have the fun task to figure out what kind of fistula was created and if there's anything wrong with it.
Besides, venous insufficiency exams, AVF cases are another of my favorites, due to the simple fact that you never know what you're getting yourself into, and I LOVE that thrill lol.
Speaking about thrills, prior to starting your scan ALWAYS palpate the area of access for that thrill. This will give you so much information even before you start scanning.
By simply doing that, you will know two important things:
Where the inflow anastomosis is located and
If the AVF is working adequately
If the fistula is patent you should be able to feel a strong and steady thrill. If you aren't able to feel it then the fistula is likely thrombosed or failing.
In this blog, we will start by reviewing the type of fistulas that could be created, protocol, technique, and criteria.
*Note: this protocol/criteria may vary from facility to facility, below is what I personally do. However, this can serve as a baseline for those of you that currently do not have a protocol in place.
Types of Arteriovenous Fistulas and Grafts
Types of Arteriovenous Fistulae

Side of artery to side of vein
Side of artery to end of vein (Brescia-Cimino AVF) (Most Common)
End of artery to side of vein
End of artery to end of vein
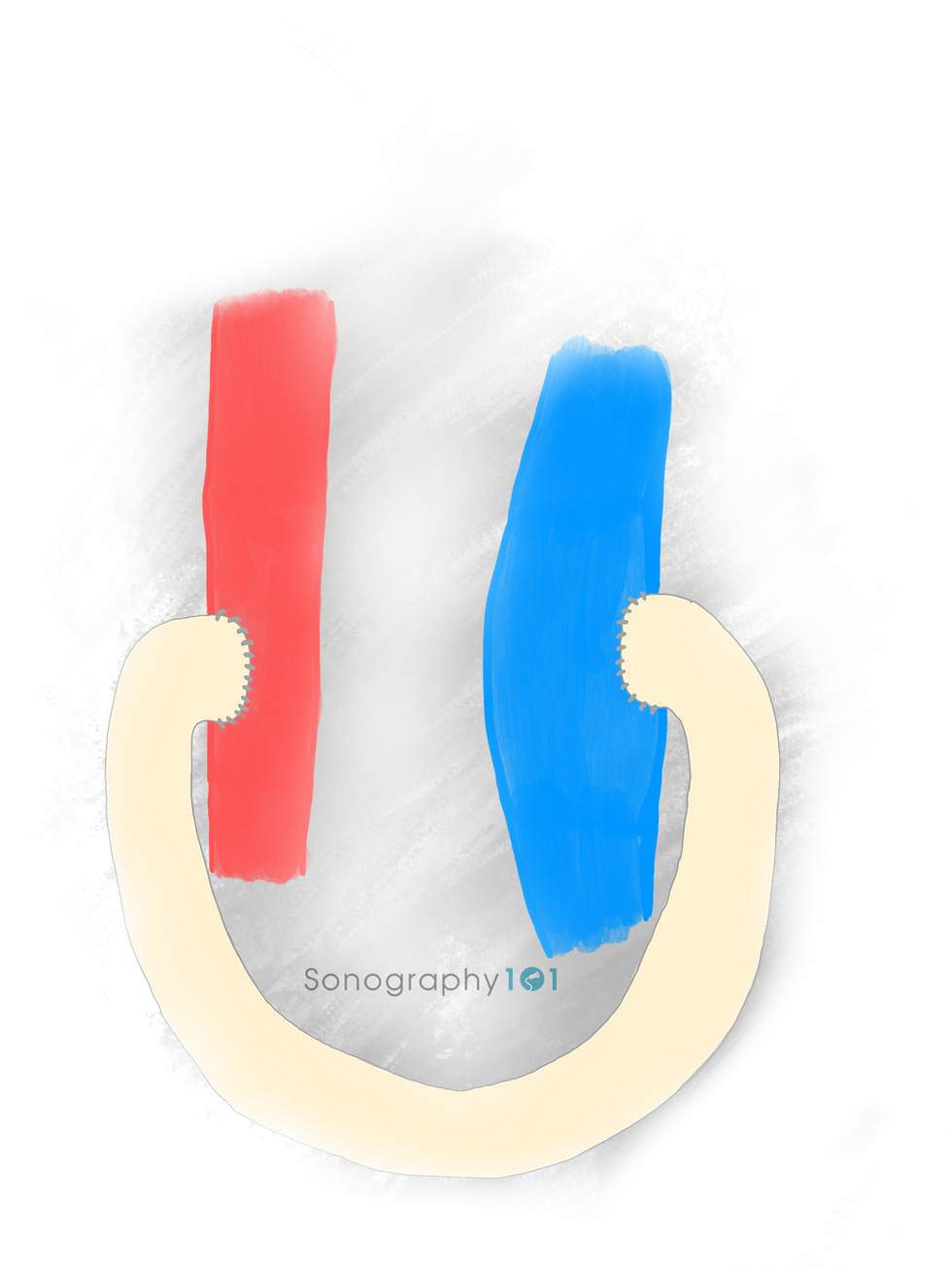
Types of A-V Grafts
Straight graft
Loop graft
Possible Connections
Forearm AVF
Radial artery to cephalic vein
Radial artery to basilic vein
Radial artery to other suitable vein (transposition)
Upper arm AVF
Brachial artery to cephalic vein
Brachial artery to basilic vein
Brachial artery to other suitable vein (transposition)
Forearm graft
Brachial artery and antecubital vein (loop graft)
Upper arm graft
Brachial artery and high brachial or basilic vein
Thigh graft
CFA to CFV
Protocol
Before starting to document your images, find out what type of fistula your patient has. If the patient does not know, then, simply sweep through to find out, once you're sure of what you're dealing with, start your protocol. The reason for this is that you don't want to start scanning with your labels saying AVF when in reality is an AVG or say it's a brachio-cephalic when in reality it's a brachio-basilic. This will save you some time, and you will feel more confident throughout your scan.
Arteriovenous Fistula (If located in the Upper Arm)

Arterial Inflow
Velocity (cm/s)
Inflow Anastomosis
Velocity (cm/s)
Upper Arm Fistula Inferior
Velocity (cm/s)
Depth (mm)
Diameter (mm)
Upper Arm Fistula Mid
Velocity (cm/s)
Depth (mm)
Diameter (mm)
Volume Flow (mL)

Upper Arm Fistula Superior
Velocity (cm/s)
Depth (mm)
Diameter (mm)
Axillary Vein
Velocity (cm/s)
Subclavian Vein
Velocity (cm/s)
*If the fistula is located in the forearm, it is the same concept, simply change "upper arm" to "forearm" in your protocol.
*Obtain velocities were "X's" are located.
Arteriovenous Graft (if located in the Upper Arm)

Arterial Inflow
Velocity (cm/s)
Inflow Anastomosis
Velocity (cm/s)
Upper Arm Graft Inferior
Velocity (cm/s)
Depth (mm)
Diameter (mm)
Upper Arm Graft Mid
Velocity (cm/s)
Depth (mm)
Diameter (mm)
Volume Flow (mL)

Upper Arm Graft Superior
Velocity (cm/s)
Depth (mm)
Diameter (mm)
Outflow Anastomosis
Velocity (cm/s)
Axillary Vein
Velocity (cm/s)
Subclavian Vein
Velocity (cm/s)
*If the graft is located in the forearm, simply change "upper arm" to "forearm". If it is a loop graft in the thigh, then change it from "upper arm" to "thigh". Also, always document whether it is a straight graft or looped graft.
*Obtain velocities were "X's" are located.

Technique
How to Measure the Volume Flow:
*Keep physics in mind in order to make sense of this calculation. Take a look at the formula ->
1. Make sample gate as big as the vessel
2. Angle parallel to the vessel (≤ 60° angle correct )
3. Measure AP diameter perpendicular to angle,
inner to inner (will kind of look like a plus sign + )

How to measure the depth: distance from skin to anterior wall of draining vein
How to measure the diameter: inner wall to inner wall of draining vein
Additional tips: Document aneurysmal dilatations, abscesses, hematomas, seromas, and stenosis. If stenosis present measure original lumen and residual lumen within the area of stenosis, as imaged below.

Criteria
6-8 weeks after surgery should meet the 3 following criteria
AP diameter of draining vein - at least 4 mm
Distance from the skin to the anterior wall of the draining vein - less than 5mm
Flow volume - at least 500 mL/min
Normal Findings:
Increased monophasic flow in feeding artery
Perivascular tissue vibration (thrill) in area of anastomosis
Increased monophasic, pulsatile flow within vein (arterialized vein)
Volume flow >500mL/min
Volume Flow Criteria
Normal value
Forearm fistula: 600 - 800
Upper arm fistula: 900 - 1200
Mature fistula: ≥500
High risk of occlusion:
AVF: <300
Graft: <650
High-output cardiac failure
Adult: >3.000
Children: >700
I hope you all enjoyed this blog,
Daryan Garcia, B.S, RDMS, RVT
P.S. Feel free to share your thoughts, your feedback is truly valuable.
References
Robbin, M.L., et al. (2002). Hemodialysis arteriovenous fistula maturity: US evaluation. Radiology. 225(1):59-64. DOI: 10.1148/radiol.2251011367.
Singh, P., et al. (2008). Clinically immature arteriovenous hemodialysis fistulas: effect of US on salvage. Radiology. 246(1):299-305. DOI: 10.1148/radiol.2463061942.
Schäberle, W. (2011). Ultrasonography in Vascular Diagnosis. Springer-Verlag Berling Heidelber.
Pellerito J., Polak, J. (2012). Introduction to Vascular Ultrasonography. Saunders.




Comments